You’ve just undergone a hysterectomy, a surgery that removes your uterus. You’re recovering, feeling a mix of relief and anxiety. Then, a new concern arises: whispers of pelvic floor dysfunction following the surgery. Is it true? Can a hysterectomy really cause issues with your pelvic floor muscles, the unseen heroes of your bladder and bowel control? The answer, unfortunately, is yes, but there’s much more to the story.

Image: www.reddit.com
Understanding the intricate relationship between your uterus, pelvic floor muscles, and the potential impact of hysterectomy is crucial for your overall well-being. This article delves into the intricacies of this connection, exploring how hysterectomy can lead to pelvic floor dysfunction and providing essential information about prevention and management.
The Pelvic Floor: An Unsung Hero
Imagine a hammock of muscles stretching across the base of your pelvis. That’s essentially your pelvic floor. It’s a complex network of muscles, ligaments, and tissues that support your bladder, uterus, rectum, and other vital organs. It plays a crucial role in:
- Urinary and fecal continence: Your pelvic floor muscles contract and relax to control the flow of urine and feces.
- Sexual function: These muscles contribute to sexual arousal and sensation.
- Support for internal organs: They act like a sling to hold your organs in place, preventing prolapse, or the sagging of organs.
Hysterectomy and Pelvic Floor Dysfunction: The Link
While a hysterectomy removes the uterus, it can affect nearby structures, potentially impacting the pelvic floor. Here’s how:
1. Surgical Trauma
The surgical incision and manipulation of tissues during a hysterectomy can injure pelvic floor muscles and nerves, leading to weakness, lack of coordination, and dysfunction. The extent of tissue trauma varies depending on the type of hysterectomy – abdominal, vaginal, or laparoscopic surgery.
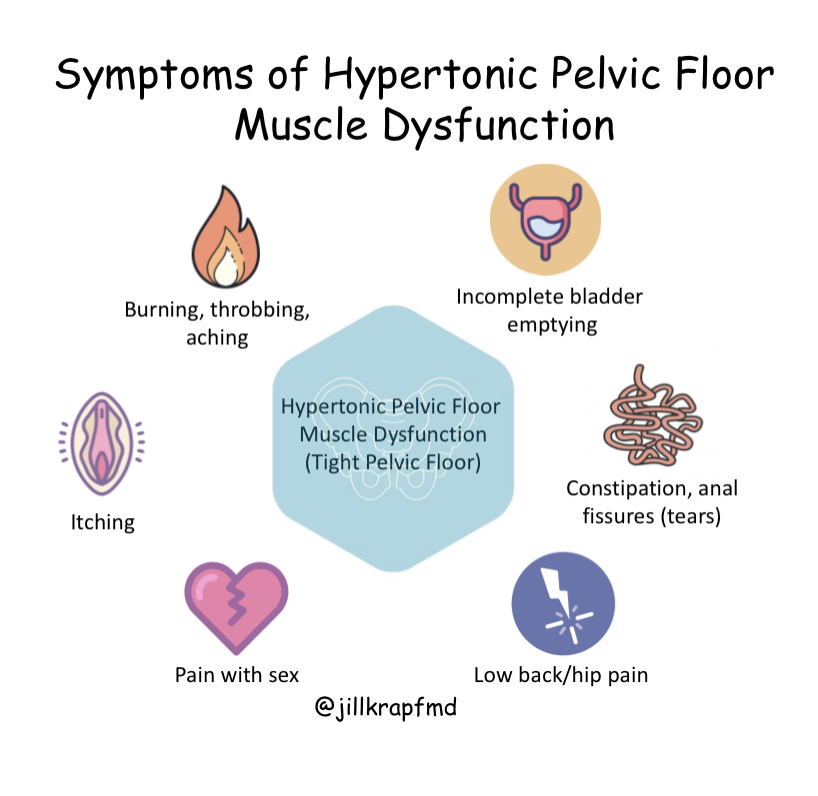
Image: jillkrapfmd.com
2. Changes in Pelvic Anatomy
Removing the uterus can alter pelvic support, affecting the muscles and ligaments that surround it. This change can directly impact pelvic floor function, leaving it less able to effectively support organs and control their function.
3. Hormonal Shifts
Hysterectomy, especially if it involves removing the ovaries, can cause a decrease in estrogen, a hormone that plays a vital role in maintaining pelvic floor muscle health and elasticity. This hormonal shift can contribute to muscle weakness and increased risk of pelvic floor problems.
Common Pelvic Floor Dysfunctions after Hysterectomy
Several conditions can develop after hysterectomy, impacting your quality of life. The most common include:
1. Urinary Incontinence
Involuntary urine leakage can occur due to weakened pelvic floor muscles, affecting your ability to control your bladder. This can range from occasional leakage during coughing or sneezing to more severe cases where urine runs constantly.
2. Fecal Incontinence
Similar to urinary issues, fecal incontinence involves accidental bowel movements due to weakened pelvic floor muscles unable to maintain control. It can range from occasional leakage to difficulty controlling bowel movements.
3. Pelvic Organ Prolapse
This occurs when your bladder, uterus, or rectum sags or drops down into your vagina, causing symptoms like pressure or a feeling of fullness, discomfort, and in some cases, leakage. It’s often caused by weakened pelvic floor muscles that can’t maintain proper support.
4. Pain and discomfort
Pelvic pain, discomfort during sexual activity, and pain during bowel movements can occur due to muscle tension, nerve damage, and weakened support after hysterectomy.
Prevention Strategies: Protecting Your Pelvic Floor
You can take steps before and after surgery to minimize the risk of pelvic floor dysfunction. These include:
1. Pre-operative Pelvic Floor Exercise
Strengthening your pelvic floor muscles before surgery can help prepare them for the potential stress of the procedure. Consult a physical therapist for personalized exercises and guidance.
2. Minimally Invasive Surgery
Laparoscopic hysterectomy, when possible, involves smaller incisions and less tissue manipulation, potentially reducing the risk of pelvic floor injury.
3. Post-Operative Recovery
Listen to your body, rest when needed, and follow your doctor’s instructions carefully for optimal recovery. Avoid heavy lifting and straining.
Management and Treatment
If you experience pelvic floor dysfunction after hysterectomy, there are effective management and treatment options. These may include:
1. Pelvic Floor Physical Therapy
A highly effective treatment approach, pelvic floor physical therapy involves customized exercises to strengthen and re-educate the pelvic floor muscles, improving control over bladder and bowel function and reducing prolapse symptoms.
2. Medications
Depending on the specific condition, medications may be prescribed to manage symptoms like urinary incontinence and pain.
3. Surgical Intervention
In certain cases, surgery may be considered to repair prolapse or other structural issues contributing to pelvic floor dysfunction.
4. Lifestyle Modifications
Changes in your lifestyle can contribute to better pelvic floor health. These include:
- Weight management: Being overweight or obese can put extra strain on your pelvic floor.
- Healthy bowel habits: Regular bowel movements help prevent straining, which can worsen pelvic floor issues.
- Avoiding smoking: Smoking weakens connective tissue, including those in the pelvic floor, increasing the risk of prolapse and other issues.
Can A Hysterectomy Cause Pelvic Floor Dysfunction
Living well after hysterectomy
It is essential to be aware of the potential for pelvic floor dysfunction after a hysterectomy. By taking steps to prevent problems, seeking prompt treatment, and utilizing available resources, you can regain control of your pelvic floor and experience a fulfilling life. Remember, you are not alone. Open communication with your doctor and a proactive approach to your health are vital for a successful recovery and a strong pelvic floor.






