The journey to motherhood is often filled with unexpected twists and turns. For many women, a C-section becomes a necessary part of their birthing experience, offering a safe and healthy delivery for both mother and baby. But what many women don’t realize is that this surgical procedure can have long-term implications beyond the immediate recovery period. One such implication that is gaining increasing attention is the potential for pelvic floor dysfunction.
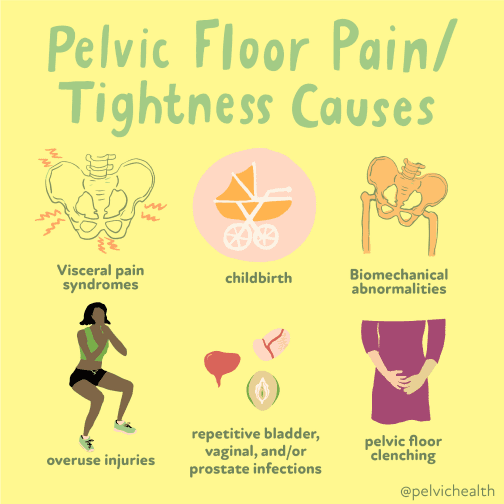
Image: viewfloor.co
As a new mom myself, I remember the anxieties that came with recovering from my C-section. While the physical pain was manageable, I soon discovered that I was experiencing new and strange sensations in my pelvic region. Urinary leakage, a feeling of pressure, and even a sense of disconnect between my body and my core muscles became my daily reality. It wasn’t until I sought out a pelvic floor therapist that I learned these symptoms were directly linked to the trauma of my C-section. This realization led me down a rabbit hole of research, determined to understand how a surgical delivery could impact such a vital part of my body.
Understanding Pelvic Floor Dysfunction
The pelvic floor is a hammock-like structure of muscles, ligaments, and tissues that forms the base of the pelvis. It is responsible for a myriad of important functions, including supporting the bladder, uterus, and rectum, controlling bowel movements, and maintaining sexual function. When this delicate system is weakened or damaged, it can lead to a range of conditions known collectively as pelvic floor dysfunction.
Pelvic floor dysfunction can manifest in a variety of ways, including urinary incontinence, fecal incontinence, pelvic organ prolapse, pain during intercourse, and chronic pelvic pain. While these symptoms can be caused by a number of factors, such as childbirth, aging, and obesity, C-sections are increasingly recognized as a contributing factor.
The Link Between C-Sections and Pelvic Floor Dysfunction
While vaginal birth can also put strain on the pelvic floor, C-sections present unique challenges that can contribute to dysfunction. Here are some of the key factors to consider:
Surgical Trauma
The incision made during a C-section can directly affect the pelvic floor muscles, potentially causing damage or weakening. The surgical manipulation of the uterus and surrounding tissues can also disrupt the normal anatomy of the pelvic floor, leading to dysfunction.
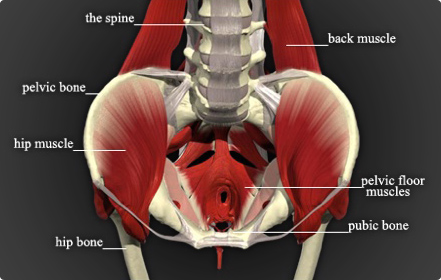
Image: clickhowto.com
Recovery and Scar Tissue
The recovery process following a C-section can be prolonged and may involve limitations on physical activity. This restricted movement can further weaken the pelvic floor muscles, making them more susceptible to dysfunction. Additionally, the formation of scar tissue from the incision can restrict muscle movement and contribute to discomfort and pain.
Postoperative Pain and Medication
The pain management medications often prescribed after a C-section can have side effects that exacerbate pelvic floor dysfunction. These medications can relax the pelvic floor muscles, leading to increased urinary leakage and fecal incontinence. The discomfort from the incision and the postpartum recovery period can also cause women to avoid engaging in pelvic floor exercises, further hindering muscle strength.
Hormonal Changes
Hormonal fluctuations during pregnancy and postpartum can also play a role in pelvic floor dysfunction. These changes can affect the strength and elasticity of the pelvic floor muscles, making them more prone to strain and damage.
Tips and Expert Advice for Managing Pelvic Floor Dysfunction
While a C-section may increase the risk of developing pelvic floor dysfunction, there are steps you can take to minimize your risk and manage existing symptoms.
1. Consult a Pelvic Floor Therapist
A pelvic floor therapist is a specialized healthcare professional who can assess your pelvic floor muscles and provide personalized treatment plans. They can teach you exercises to strengthen and rehabilitate your pelvic floor, as well as offer strategies to manage urinary incontinence and other symptoms.
2. Engage in Regular Pelvic Floor Exercises (Kegels)
Kegel exercises are essential for strengthening and toning the pelvic floor muscles. To perform Kegels, imagine you are trying to stop the flow of urine or hold back gas. Contract your pelvic muscles for a few seconds, then relax. Repeat this exercise several times a day, gradually increasing the duration and intensity of the contractions.
3. Maintain a Healthy Weight
Excess weight puts additional strain on your pelvic floor, increasing the risk of dysfunction. If you’re carrying extra weight, losing even a small amount can have a positive impact on your pelvic floor health.
4. Avoid Straining and Heavy Lifting
Activities that involve straining, such as heavy lifting, constipation, and prolonged coughing, can put undue stress on your pelvic floor. Be mindful of these activities and modify them if necessary to reduce strain.
5. Practice Good Bowel Habits
Constipation can put extra pressure on your pelvic floor, making it more susceptible to dysfunction. Regular bowel movements are important for maintaining pelvic floor health. Eat a high-fiber diet, stay hydrated, and incorporate regular exercise to encourage healthy bowel function.
Pelvic Floor Dysfunction FAQ:
What are the common signs and symptoms of pelvic floor dysfunction?
Common symptoms include urinary incontinence, fecal incontinence, pelvic organ prolapse, pain during intercourse, and chronic pelvic pain. It is crucial to remember that these symptoms can have varied causes, and a comprehensive evaluation by a healthcare professional is necessary for accurate diagnosis.
Can pelvic floor dysfunction be treated?
Yes, pelvic floor dysfunction can be treated effectively. A pelvic floor therapist can provide individualized treatments that may involve exercises, biofeedback, electrical stimulation, or other modalities. Depending on the cause and severity of dysfunction, other medical interventions may also be required.
Can I prevent pelvic floor dysfunction after a C-section?
While you can’t completely eliminate risk, there are steps you can take to minimize the likelihood of developing pelvic floor dysfunction after a C-section. These include engaging in early mobilization, following your doctor’s recommendations for recovery, performing regular Kegel exercises, and seeking guidance from a pelvic floor therapist.
What should I do if I suspect I have pelvic floor dysfunction?
If you are experiencing any symptoms of pelvic floor dysfunction, it is essential to consult your doctor or a pelvic floor therapist promptly. These healthcare professionals can help you understand the potential causes of your symptoms and guide you toward appropriate treatment.
Can C Section Cause Pelvic Floor Dysfunction
Conclusion:
Pelvic floor dysfunction can be a challenging condition to navigate, but it is important to know that you are not alone. Learning to identify risk factors, understand the ways a C-section can impact your pelvic floor, and proactively engaging in preventive measures and treatment can empower you to take control of your recovery and long-term health.
Are you interested in learning more about pelvic floor dysfunction and how to manage its impact after a C-section? Share your thoughts and experiences in the comments below and join the conversation!






